Atopic Dermatitis On The Scalp: Causes & Symptoms
Atopic dermatitis. The term sounds complex, medical, and maybe a bit terrifying.
But in reality, atopic dermatitis (AD) is simply the most common cause of eczema - red, itchy skin. That’s it. So, if you think you might have atopic dermatitis, don’t panic - there’s a lot to learn, and nothing to be afraid of. Let’s brush up on one of the most commonly diagnosed skin conditions, and how it relates to dandruff.
What is atopic dermatitis?
Atopic dermatitis, also known as atopic eczema, is a skin disease that causes chronic itching and scaly skin. It’s an inflammatory skin disorder, and it’s not contagious. Classically, it is a chronic type of eczema that waxes and wanes over time, and statistics from the National Eczema Association show that its prevalence is increasing worldwide.
Flare-ups result from exposure to specific environmental factors or even foods. From a house dust mite to harsh laundry detergents, nearly anything can be a trigger for eczema. Atopic dermatitis often coexists with other allergic diseases, including hay fever (allergic rhinitis), asthma, a lack of the protein filaggrin, and migraines. The most typical atopy associated with atopic dermatitis is the triad of atopic eczema, asthma, and allergies.
Fortunately, treatments are available that penetrate the skin barrier and help prevent recurring flare-ups. (We’ll get to that shortly.)
What are the symptoms of atopic dermatitis?
Symptoms of atopic dermatitis range from mild to severe, and they can present differently in people of different ages. Plus, if you have food allergies or any other type of allergy, your AD might get worse with exposure.
You might notice redness, thickened skin, and other related symptoms with eczema. You may experience skin infections from itching to crusting patches and hives. According to the American Academy of Dermatology, 90 percent of people with this atopic disease are diagnosed before they reach five years of age. Pediatric patients are at an increased risk of skin infection, as young children and older children are both more likely to pick at their rashes. Chronic rubbing can also cause a thickening of the affected area called lichenification. Common areas where the eczema rash crops up include the creases of your elbows and the backs of your knees. Eczema can also appear on the lip as eczema herpeticum. However, you might experience itching and eczematous skin anywhere on your body, including on your scalp, which may result in dandruff.
The atopic dermatitis-dandruff connection
If you’ve been noticing dandruff flakes, you might be wondering: could this be related to atopic dermatitis? The short answer is yes.
Dandruff is simply the flaking that results from irritation of the scalp. And that irritation can be caused by atopic dermatitis (as well as other conditions like seborrheic dermatitis and psoriasis). In other words, when your scalp is chronically itchy (atopic dermatitis) it may start shedding flakes that end up in your hair and on your clothing (dandruff).
Not everyone with AD has dandruff, and not everyone with dandruff has AD. But the conditions are often linked.
Other conditions related to atopic dermatitis
As our body’s largest organ, the skin can get irritated and itchy for any number of reasons. In other words, there are many triggers for atopic dermatitis. There are also many secondary infections that commonly occur in atopic dermatitis patients such as staphylococcus. And, there’s a slew of health issues that may be confused with AD but which are actually quite different. Let’s review some of these related conditions:
Other common dermatitis conditions
Pruritus is a fancy term for general itching. The catch-all term refers to itching from every cause that’s not a disease like sunburns, bug bites, or plain old dry skin.
Keratosis pilaris (KP) is another common condition. KP presents as dry, rough skin with small bumps centered on hair follicles. It can be chronic or lifelong and happens when your skin produces too much keratin, causing skin that’s bumpier than usual.
Contact dermatitis is related to atopic dermatitis in that it’s another form of eczema or skin irritation. But contact dermatitis is a typical rash that happens when you encounter an irritant – irritant contact dermatitis, or an allergen – allergic contact dermatitis. For example, you could be sensitive or allergic to a fragrance, ingredient, plant, or other material. Contact with an irritant or allergen results in red, itchy and sometimes blistering skin.
Nummular dermatitis or nummular eczema presents similarly to eczema but also involves skin lesions the size and shape of a coin.
How is atopic dermatitis diagnosed?
Many people with atopic eczema self-diagnose after browsing online resources. But consulting a physician is always a smart step. A healthcare practitioner will examine your skin, ask you about your symptoms, and offer a diagnosis.
During your visit, the doctor will ask questions about your family history and any existing allergies. Most of the time, examining your skin gives the doctor the information they need to make an official diagnosis. If an allergy is expected, you may undergo patch testing to identify the culprit allergens, or possibly even a skin biopsy to rule out other potential issues.
...when your scalp is chronically itchy (atopic dermatitis) it may start shedding flakes that end up in your hair and on your clothing (dandruff).
What treatments work for atopic dermatitis?
Treatment of atopic dermatitis starts with creams, salves, and lotions that are gentle on your skin and help it heal. A dermatologist may also recommend bleach baths, biologics, or phototherapy with ultraviolet light to help manage atopic dermatitis symptoms. Many include anti-inflammatory agents, which help reduce swelling and redness, and moisturizing ingredients, which help your skin to replenish itself. For example:
Topical corticosteroids are topical steroids that you apply to your skin to reduce inflammation and improve the redness and associated itching and irritation. Commonly, topical corticosteroids come in the form of a cream, ointment, or gel prescribed by your doctor.
Topical anti-inflammatory products block enzymes to prevent your body from having an excessive immune response to irritants. For example, topical calcineurin inhibitors stop your body from using its own calcineurin to activate the T-cells in your immune system. Calcineurin inhibitors lessen inflammation by convincing your body that there’s no threat to your immune system. Topical anti-inflammatories include over the counter gels, gel patches, creams, and ointments. There are also stronger topical anti-inflammatories that may be prescribed by your doctor.
Skin barrier creams are often helpful in treating all forms of eczema and can help to relieve itching and reduce the potential for subsequent flare-ups. But be careful when selecting a product as some may contain ingredients that can further aggravate your skin irritation, and it might take trial and error to figure out the best solution. While often found in the drugstore, many cosmetic and skincare brands also offer skin barrier creams, salves, and ointments.
Treatments for seborrheic dermatitis
While topical creams can help relieve itching and scaly skin on your arms, legs, and even face, they don’t help your scalp. Many people with atopic dermatitis have skin and scalp challenges - seborrheic dermatitis, which can cause dandruff.
If you treat the rest of your skin but skip your scalp, you could wind up with dandruff (never a fun outfit accessory) and maybe even hair loss or permanent hair follicle damage over time. So, what to do with atopic eczema on your head?
Medicated dandruff shampoos are perfect for the job. Shampoos containing Zinc Pyrithione (ZPT) fight dandruff on a molecular level by reducing the fungus that commonly causes dandruff.
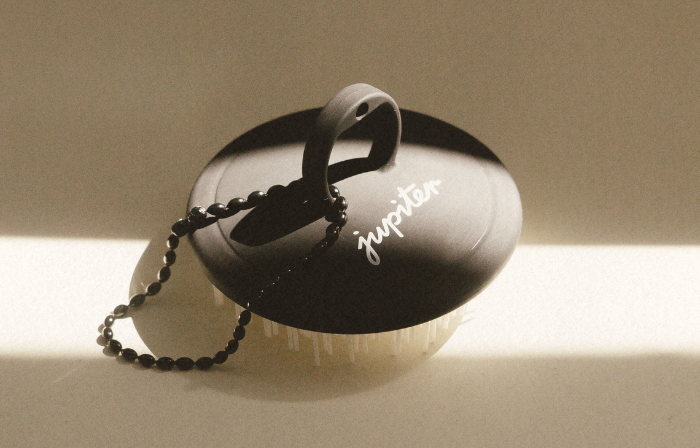
Jupiter’s Balancing Shampoo is formulated with Zinc Pyrithione to cleanse your scalp and eliminate flaking. Pair it with our Restoring Serum, also formulated with Zinc Pyritihione, and you’ve got an effective dandruff treatment that will help stop your flakes for good and improve your quality of life.
Other important steps for dealing with AD
Creams, antihistamines, and medications prescribed by your dermatologist can help address your symptoms and improve your barrier function. But you’ll likely continue to experience flare-ups of atopic dermatitis unless you address its underlying causes such as allergic reactions, dryness, or sweat build-up. Many environmental triggers can cause your AD to worsen, so taking these preventive steps could help avoid outbreaks:
Take cooler showers to avoid inflaming your skin even more. Dry skin is stripped of natural oils and hot showers exacerbate this. Heat opens your pores, too, allowing potential pathogens to get inside.
Avoid environmental triggers such as pet dander, outdoor allergens, dust mites, and cigarette smoke.
Wear loose-fitting clothing and try to avoid intense sweating in non-breathable fabrics. Rinsing with a cool shower immediately after you exercise can help keep your pores clean.
Check your personal care products for irritants. Cosmetic shampoos, conditioners, hand soaps, body washes, makeup, skin cleansers, perfumes and colognes, lotions, moisturizers, and many other personal products can contain irritating ingredients. You’ll find dyes, fragrances, comedogenic oils, and other unhealthy components for eczematous skin on many labels.
Inspect your household products for irritants. Things like laundry detergent, fabric softener, dish soap, hand sanitizer, and cleaning products may trigger or worsen your condition.
Next steps for living with atopic dermatitis
While there isn’t always a clear explanation for why people get atopic dermatitis, there are ways to treat the symptoms and enjoy clearer skin and a flake free scalp. Addressing all aspects of your skin condition can help keep atopic dermatitis flare-ups, and its unwanted side effects, at bay.

Meet our head honcho. This soothing multi-tasker gets to the root of flaking and irritation, thanks to our star active ingredient, Zinc Pyrithione. Backed by a lush aroma of mint, vanilla, rosemary, sage, tangerine, and lavender, it’s bound to elevate your mood, and your shower.